NEWS RELEASE July 2020
Are Cloth Masks Aerosol Generators?
The advice to use a mask to fight COVID is like saying use a knife for surgery. Who cares whether it is a butcher knife of a high quality scalpel? In both cases life hangs in the balance of the product choice.
Most everyone now agrees that a mask is a major weapon in the COVID battle. It is therefore imperative that we use the right product. It can be argued that efficient masks will save seven times as many lives as inefficient masks. This important theory will be reviewed continually in the Coronavirus Technology Solutions daily alerts and will be one of the subjects discussed in our August 20 webinar.
There is now a mountain of evidence that a significant quantity of the COVID-19 virus travels through the air in small aerosols. A cloth mask will allow most of these particles to pass through. An N95 Mask will capture 95% or more of them. One commonly stated estimate is that coughs and sneezing are responsible for 60% of the transmission, contact 20% and aerosols 20%.
The main benefit of a cloth mask is that it will theoretically prevent the 60% transmitted by coughing or sneezing larger droplets. What if this is not true and instead the cloth mask acts as an efficient aerosol generator converting large droplets on the mask interior into small droplets discharged into the atmosphere?
There are many studies documenting how a large droplet evaporates and creates small droplets. However, a droplet on the interior of a mask is ideally situated to be converted to aerosols by the passing of air around or through it. One of the air pollution control scrubber designs uses a screen. Droplets containing surfactants are sprayed on the back of the screen. Dirty air then moves through the screen forming small bubbles. Could this be what happens to cough and sneeze droplets?
Investigators with the Ulsan College of Medicine, Seoul, South Korea. published a research letter, in the Annals of Internal Medicine, analyzing the virus emission during coughing while wearing a surgical or cloth mask. The paper was later retracted due to questions about the mathematics but some of the findings are important in answering the question as to whether a cloth mask can be an aerosol generator.
The research letter states. “All swabs from the outer mask surfaces of the masks were positive for SARS–CoV-2, whereas most swabs from the inner mask surfaces were negative.”
The research letter investigators found greater contamination on the outer surface of the face masks than on the inner surfaces.
“Although it is possible that virus particles may cross from the inner to the outer surface because of the physical pressure of swabbing, we swabbed the outer surface before the inner surface,” the research letter states. “The consistent finding of virus on the outer mask surface is unlikely to have been caused by experimental error or artifact.”
If some virus moves from the inner to outer surface it stands to reason that some quantity traveled from the inner surface into the ambient air. There is no doubt that water vapor from the droplet moves through the mask. Why wouldn’t the virus move through along with it?
There are many experts better qualified to answer these questions than is the McIlvaine Company. But there is enough evidence of aerosol generation from cloth masks that answers are necessary.
If cloth masks are aerosol generators they are relatively ineffective in fighting COVID. They allow 80% of the virus to be transmitted where N95 allows 12%.
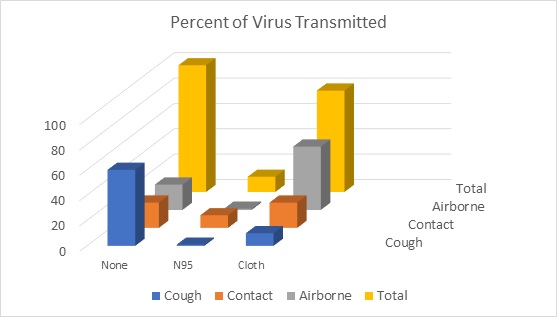
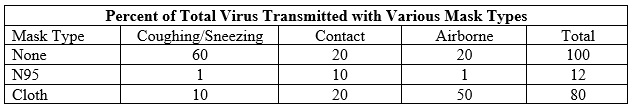
The assumption Is that both transmitter and recipient are wearing the same mask type. So in the case of the N95 mask there would be less escaping virus to contaminate surfaces. This should result in a 50% decrease in contact transmission. The difference in numbers of infections would be reduced seven fold as compared to cloth masks. The number of deaths reduced could even be greater. Evidence indicates that aerosols penetrate the lungs and cause more serious damage than do viruses in the nasal passages.
We expect a lively debate on this subject during our August 20 webinar. We invite anyone to send opinions or evidence in advance and to participate in the webinar. Details are found at: http://home.mcilvainecompany.com/index.php/2-uncategorised/1574-coronavirus-webinars
Bob McIlvaine can answer your questions at 847 226 2391 This email address is being protected from spambots. You need JavaScript enabled to view it.
